A study conducted at Cambridge University found antibiotic-resistant E. coli bacteria on 24% of chicken samples taken from the seven largest supermarkets in the United Kingdom, according to the Center for Infectious Disease Research and Policy at the University of Minnesota (CIDRAP). That is more than four times higher than results obtained in another study conducted in 2015. Resistance was “frequently found to three families of antibiotics that are particularly important for treating human E. coli urinary-tract and blood-poisoning infections,” according to the study.
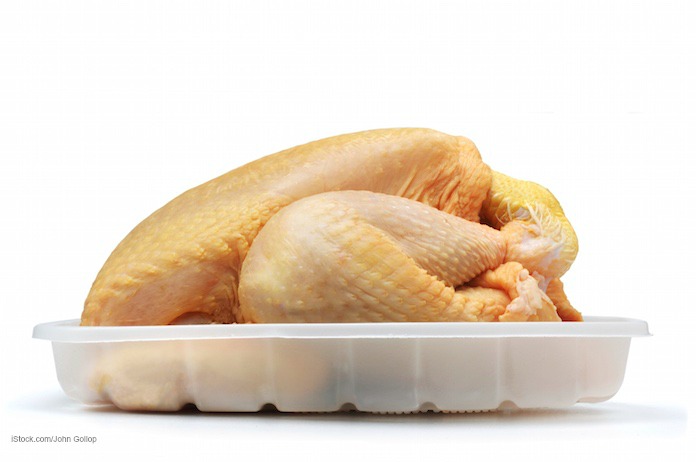
The study was commissioned by the Alliance to Save Our Antibiotics, an organization in England that is dedicated to reducing the prevalence of antibiotic-resistant bacteria in our food supply. Scientists analyzed 189 pork and poultry samples that were produced in the U.S. and purchased at seven of the U.K.’s largest supermarkets, including Sainsbury’s, Tesco, Waitrose, Aldi, and Morrisons.
Researchers discovered that 24% of the chicken samples tested positive for “extended spectrum beta-lactamase (ESBL) E. coli,” an isolate that is resistant to cephalosporin antibiotics. That’s the kind of antibiotic used to treat E. coli infections in the blood and urinary tract. The study also revealed that 51% of the E. coli in the pork and poultry samples was resistant to trimethoprim, an antibiotic used to treat lower urinary tract infections. Nineteen percent of the E. coli was resistant to gentamicin, an antibiotic used to treat upper respiratory tract infections. None of the E. coli isolates were resistant to fluoroquinolones or colistin.
And the study found that E. coli bacteria were isolated from 98% of the meat samples. No pork samples tested positive for ESBL E. coli.
This is the first study of levels of antibiotic resistance in E. coli found in supermarket meat sold in the UK. The findings suggest that some of the bacterial antibiotic resistance to key antibiotics is coming from farm animals. The strongest evidence for antibiotic resistant transfer from farm animals to people has been for bacteria such as Salmonella, but this study is evidence that resistance in human E. coli infections is partly of farm-animal origin.
Trimethoprim is given to farm animals through their feed and water. And cephalosporins and gentamicin are used off-label in that country to treat infections in farm animals.
Emma Rose of the Alliance to Save Our Antibiotics said in a statement, “these findings show the level of antibiotic resistance on retail meat to be worse than expected. Supermarkets must now publicly commit to policies which prohibit the routine mass-medication of groups of healthy animals, and take immediate steps to reduce farm use of the ‘Critically Important’ drugs.”
Data from Public Health England, according to the study, shows that E. coli infections kill more than 5,500 people a year in England alone. That is more than twice as many as those killed by MRSA and Clostridium difficile infections combined. The study also mentions that “no genuinely new antibiotics for treating E. coli infections have been discovered for over 35 years,” so the need to protect the effective antibiotics we do have is critical.
These are not the type of E. coli infections that are caused by food poisoning; they are called extra-intestinal E. coli infections. But since the treatment of food animals seems to be contributing to E. coli antibiotic resistance, the way farmers treat their food animals can make a difference in human health and disease.