There is an ongoing controversy in the medical community about the safety of platelet transfusions in patients who have platelet consumptive disorders like hemolytic uremic syndrome (HUS), but an analysis of patients with E. coli O104:H4 infections who developed HUS suggests that platelet transfusions may be safe in adult HUS patients (Benke). Previous studies have suggested that platelet transfusions may be harmful to patients who have thrombotic thrombocytopenia purpura (TTP), another platelet consumptive disorder very similar to HUS.
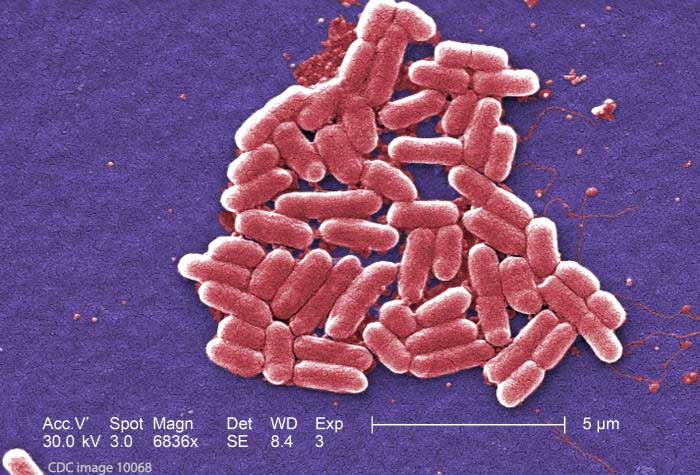
In the study, researchers analyzed an E. coli O104:H4 outbreak that occurred in Germany during the summer of 2011. Thousands were sickened in that outbreak. About 30% of those patients developed hemolytic uremic syndrome, which was triple the percentage in most E. coli outbreaks. The outbreak was eventually traced back to raw Egyptian fenugreek sprouts.
In the German outbreak, 711 patients developed HUS. Sixty-one of those patients received platelet transfusions while they were hospitalized.
The researchers looked at data for 250 of the patients who developed HUS, who met the criteria of severe thrombocytopenia with a platelet count of 50/nL or lower, admission to intensive care units, and severe hemolysis with administration of packed red blood cells. Forty-four of those patients received platelet transfusions and 205 control patients did not. Most of the patients studied were female, aged 30 to 56 years. Three children aged 5 to 18 years were part of the study group.
The transfusions were administered a median of 7 days after onset of diarrhea. After the transfusions, there was a “transient and slight increase” in inflammation parameters, but there was no significant difference in major complications such as seizures or requirement for ventilation or renal replacement therapy. Thrombotic events were relatively rare, and the mortality was not significantly different between the two groups.
Laboratory data for the group at admission included a platelet count of 81, hemoglobin levels of 12.3, and creatinine levels of 114. Platelet counts dropped below 50 n/L within six days after admission. The lowest platelet counts on the date of transfusion or one day before were 25/nL.
In the patients who received platelet transfusions, the count increased from 26/nL to 52/nL one day after the transfusion. Hemoglobin levels also increased because of a simultaneously administered red blood cell (RBC) transfusion.
Overall, the researchers did not find any association of platelet transfusion and clinical complications specific for E. coli-HUS. But they caution that regular complications of transfusions must be taken into account. There was a slight increase of inflammation parameters, since LDH levels and leukocyte count, which are markers for a worse outcome of E. coli-HUS, might slightly increase after platelet administration. They also stated that platelet infusion could enhance or prolong the activity of HUS by a minor amount.
The researchers acknowledge that a limitation of the study is that patients with E. coli-HUS are most often children, while the German outbreak patients were primarily adults. They stated that “the administration of both platelet transfusion and interventional therapy would be considered more restrictively in children.” Overall, in this particular outbreak, 6 of 711 STEC-HUS patients died of procedural-related bleeding complications after central catheter placement.
In summary, inflammatory chemistry parameters did increase slightly, but there was no significant negative impact. The researchers stated that “platelet transfusions should not be considered to be contraindicated for the treatment of bleeding or in advance of invasive procedures in STEC-patients with HUS.”
Reference: Beneke, Jan, et al. “Clinical and Laboratory Consequences of Platelet Transfusion in Shiga Toxin–Mediated Hemolytic Uremic Syndrome.” Transfusion Medicine Reviews 31.1 (2017): 51-55.




