During 2011 and most of 2012, there was a Legionnaires’ Disease (LD) outbreak at the Pittsburgh Veterans Administration hospital. Most news outlets did not report this outbreak, mainly because the VA Hospital did not report all of the cases to the National Electronic Disease Surveillance System (NEDSS), even though Legionnaires’ is a notifiable disease. In addition, the Pennsylvania Department of Health did not analyze hospital-acquired infections to look for outbreaks until the middle of last year. During the outbreak, 21 patients were sickened, and five people died. About 40% of those who acquire this illness die.
 Legionnaires’ Disease first came to public attention in 1976, when an outbreak at an American Legion convention sickened 14 people and killed 6. At that time, panic swept the country because no one knew what caused the illness and the public expected an epidemic.
Legionnaires’ Disease first came to public attention in 1976, when an outbreak at an American Legion convention sickened 14 people and killed 6. At that time, panic swept the country because no one knew what caused the illness and the public expected an epidemic.
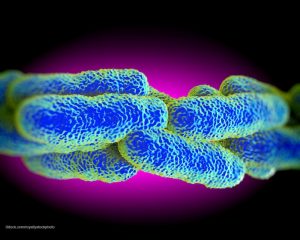
Most cases are caused by the Legionella pneumophila bacteria, which lives in water. Symptoms of Legionnaires’ Disease, which usually occur 2 to 14 days after exposure, include fever, chills, and a cough. Other symptoms include muscle aches, tiredness, headache, loss of coordination, and sometimes vomiting and diarrhea. The bacteria is transmitted through inhaling its aerosolized form from an infected water source. Legionella can travel 6 kilometers from its source. About 18,000 hospital admissions every year are related to Legionnaires’ Disease.
Last month, Senator Bob Casey (D-PA) called on the Veterans Administration to make a CDC report on the outbreak public. He said, “a public report would provide valuable information about the outbreak and the VA’s response to the families who have been impacted by this tragedy. Also, the people of southwestern Pennsylvania have a right to know what happened.”
The CDC did release testimony on their investigation that stated a highly pathogenic strain of Legionella was in the hospital’s potable water system, perhaps related to extension construction done at the time. They also state that the hospital did not recognize healthcare-associated cases of Legionnaires’ Disease for “an extended period of time”, and the cases reported to county and state public health offices were not recognized as part of an outbreak, which may be because there is a high baseline prevalence of Legionnaires’ Disease in Pittsburgh. Their recommendations included frequent testing for the bacteria at that facility, LD surveillance including strict case definition, and reevaluation of Legionella control protocols of the hospital.




