The Centers for Disease Control and Prevention has just released Untreatable, a new report all about antibiotic-resistant bacteria. The report is the “first-ever snapshot of the burden and threats posed by the antibiotic-resistant germs having the most impact on human health,” according to the report.
 Every year in this country, at least 2 million people are sickened with bacteria that are resistant to bacteria. At least 23,000 of those people die as a direct result of their infections. The urgent threats include Clostridium difficile, while serious threats include drug-resistant Campylobacter (pictured), Salmonella Typhi, and Shigella. All can be passed to human beings through food and water.
Every year in this country, at least 2 million people are sickened with bacteria that are resistant to bacteria. At least 23,000 of those people die as a direct result of their infections. The urgent threats include Clostridium difficile, while serious threats include drug-resistant Campylobacter (pictured), Salmonella Typhi, and Shigella. All can be passed to human beings through food and water.
The CDC states that if the ability to effectively treat common infections is lost, life-saving and life-improving medical advances will be useless, since those advances depend on antibiotic use. The agency has identified four core actions that must be taken: avoiding infections in the first place, tracking these infections and identifying risk factors, improving antibiotic use and stewardship, and developing new antibiotics and new diagnostic tests.
Food Poisoning Bulletin has been covering the story of antibiotic-resistant bacteria in foods for years. In July, we told you that antibiotic-resistance in Campylobacter is now between 97 and 100 percent. In June, we reported on a CDC study that showed Salmonella enterica is becoming increasingly resistant to antibiotics. And in April we reported on a study by Environmental Working Group that found antibiotic-resistant bacteria on many supermarket meats.
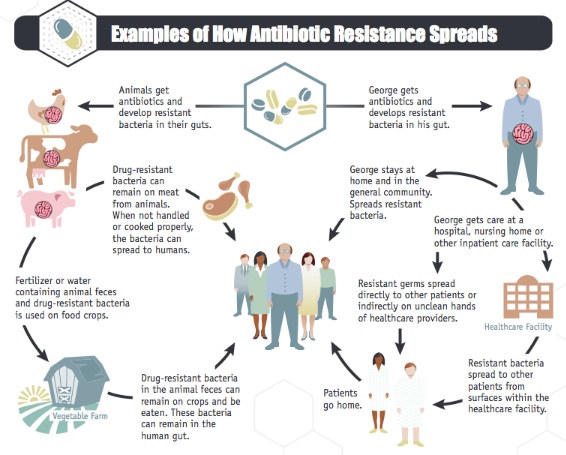
The report details the CDC’s work to prevent antibiotic resistance in food. The National Antimicrobial Resistance Monitoring System (NARMS) was established in 1996 to track resistance among bacteria commonly transmitted through food. The CDC states that “because of the link between antibiotic use in food-producing animals and the occurrence of antibiotic-resistant infections in humans, antibiotics should be used in food-producing animals only under veterinary oversight and only to manage and treat infectious diseases, not to promote growth.”
But several consumer and food safety groups have been critical of the government’s response and action in this area, including the National Resources Defense Council, which in February 2013 released a statement that found antibiotic abuse in the farm industry is on the rise. In May 2013, the Center for Science in the Public Interest scolded the USDA for not taking action on antibiotic resistant Salmonella strains found in meat. In addition, last December the FDA said it would not expand current requirements under the Animal Drug User Fee Act to report details about antibiotic sales for animal use.
For each of the drug-resistant bacteria, the report states the problem, what the CDC is doing, what you can do, advice for healthcare providers, and offers online resources. It’s worth looking over the report to see the information and advice. Drug-resistant Salmonella, for instance, causes 100,000 illnesses a year and is resistant to Ceftriaxone and Ciprofloxacin; some Salmonella bacteria are resistant to five or more antibacterial classes of drugs. To help, consumers can avoid drinking raw milk, follow safe cooking procedures, report suspected illnesses from food to health departments, don’t prepare food for others if you have a GI illness, and be especially careful preparing food for those in high risk groups.
Graphics courtesy CDC




